According to the American Institute of Stress, numerous studies show that job stress is far and away the major source of stress for American adults and that it has escalated progressively over the past few decades. So, what are leaders of companies doing to improve employee mental health at work?
In our recent webinar, Actionable Ways to Improve Workplace Well-Being, we explored how HR teams can do just that. Licensed therapist, Kristy Paterson, discussed:
- Techniques to assess existing mental health challenges in the workplace (i.e. burnout and anxiety)
- How to immediately improve the mental health of your employees for a happier, and healthier company
- The important relationship between employee mental healthcare and company success in a competitive job market amidst The Great Resignation.
Current state of mental health at work in the US
According to the CDC, many people suffering from mental health disorders also need care for other physical health conditions, including heart disease, diabetes, respiratory illness, and disorders that affect muscles, bones, and joints The costs of treating people with both mental health disorders and other physical conditions are 2 to 3x higher than for those without co-occurring illnesses. By combining medical and behavioral health care services, the United States could save $37.6 billion to $67.8 billion a year.
Stigma and access to care are the biggest hurdles to combining medical and behavioral health services. Mental healthcare has historically been an afterthought of the modern approach to healthcare for Americans. The correlation between total medical healthcare spend and behavioral health conditions in the workplace is astonishing. In this 2021 study of the prevalence of behavioral health conditions in the workplace, 10% of your workforce drives 70% of total medical spend, and over half of that 10% have a mental health condition.
Direct costs
Direct costs correlating to mental health conditions are expenses that fall under the realm of treatment. Examples of direct costs would be:
- Inpatient treatment
- Emergency room visits
- Out-patient services
- Pharmaceutical treatments
“The economic costs of mental illness will be more than cancer, diabetes, and respiratory ailments put together.” - A director of the U.S. National Institute of Mental Health at the World Economic Forum
Indirect costs
Indirect costs are the less obvious spends, and substantially more costly in the long-term for companies. These costs are the indirect effect of untreated mental health conditions (i.e. depression, PTSD, bipolar, Opioid Use Disorder, etc), such as:
- Absenteeism (i.e. sick days)
- Reduced productivity
- Disability costs
Gallup’s State of the American Workplace survey looked at how engaged US workers are in the workplace. The study found more than 64% of workers are not engaged at work “mentally checked out” as a result of stress, leading to a loss of productivity.
How to support the mental health of all employees:
This three-step guide will provide actionable ideas for you to incorporate into your company for happier, healthier employees.
1. Create an action plan
The first step in supporting employee mental health is making well-being an organizational goal.
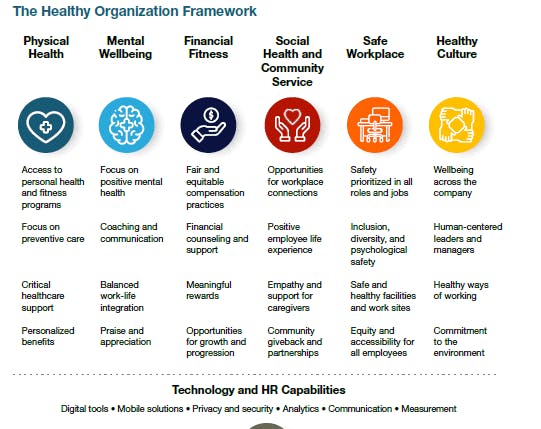
A holistic approach to your organizational goals is the best way to incorporate mental well-being, along with physical, financial, social, etc. Holistic programs create healthy organizations, which are good for business, people, and society.
The Healthy Organization provided by The Josh Bersin Company is a great example of what a healthy company goal structure looks like, and what companies consider moving towards the betterment of their current and future workforce. Cookie-cutter health plans are becoming a thing of the past, and we continue to spread awareness of the importance of healthy mental well-being.
2. Measure Employee Mental Health
There are multiple opportunities to measure employee mental health on a weekly, monthly, and quarterly basis. These include:
- One-on-Ones - These surveys allow managers to build better relationships with their employees. One-on-ones normalize the discussion around mental health, reduce stigma, and help managers determine the appropriate health programs to suggest to their direct reports.
- Employee Engagement Surveys (anonymous survey, increases trust and reduces stigma around mental health which allows you to analyze responses about how different facets are impacting employees' mental health at work)
- Pulse Surveys (quick, short surveys sent out on a monthly or quarterly basis to employees to get a general idea of current job satisfaction, communication, and effectiveness of programs, feedback on leadership, etc)
Each of these opportunities allows for feedback and should be used to guide investments in program awareness and elevate areas of concern in your organization.
3. Understand the Data
Information and data are key to understanding the impact of mental health conditions and establishing a baseline for workplace mental health initiatives. By leveraging data from your mental health platform, you can understand the true impact that the available benefits have on the organization.
Other ideas
Although these are the main three actionable ideas to implement in your organization, one of the first things that you can do to help employees is to make sure that the mental healthcare solution you offer is easy to access.
If you have an EAP or mental health platform with low usage rates, it's likely that employees are unaware of the benefit, or they don’t know how to access it. Research shows that 72% of employees want their employer to prioritize mental health and wellbeing, so it's important to make sure that they know they are supported.
Watch the full webinar on-demand here, or learn more about Cerebral for Business, and how we can support your employees’ mental health.

Telehealth and the Power to Revolutionize Access to Mental health care

How Telehealth Can Increase Access to Mental Healthcare for College Students

Age Verification and What it Means for Access to Care

Call 911 if you’re having a
mental health emergency
Text Home to 741-741 if you're in emotional
distress and need immediate support
Call or text 988 Suicide &
Crisis Lifeline. Chat service
is available at 988lifeline.org.